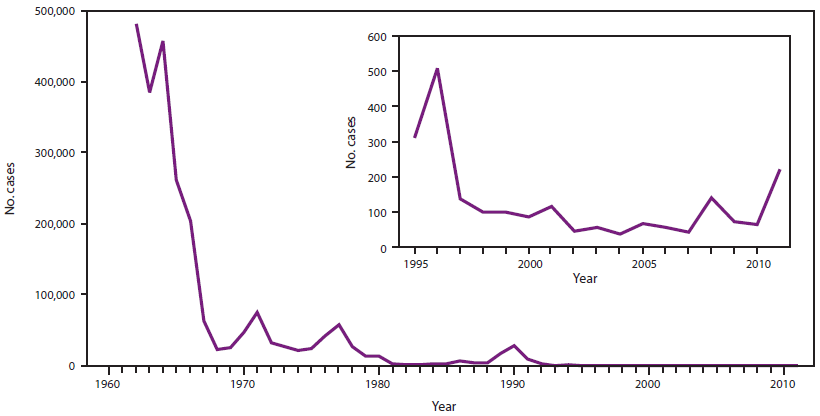
Measles used to be a major childhood disease, affecting virtually all children in dramatic
periodic outbreaks. The measles virus causes high fever, rash, runny nose, conjunctivitis, and malaise. It can also result in death. In the 1960s
a vaccine was developed, and it was ultimately merged into what became the
currently-used MMR vaccine. That vaccine helped reduce the incidence of measles to virtually non-existent levels in the US. A recent
MMWR depicts the dramatic decrease of disease after vaccine introduction:
Sadly, a
1998 report finding an association between the MMR
vaccine and autism led to decrease in the incidence of vaccination and attendant increase in measles disease (inset of the graphic). That
study was
retracted in 2010 after investigators failed
to confirm its findings. Nonetheless,
a large number of consumers continue to believe the bogus result that the MMR and other vaccines cause autism and thus forgo vaccinating their children. (There are additional reasons people do not vaccinate their children besides fear of autism; just google "why I'm not vaccinating my child" and you'll get a good sampling of those reasons.)
Recent months have seen continued transmission of measles in susceptible populations across the US, including
California and
New York City. Why is measles a problem when an effective vaccine is so commonly available? Often,
travelers become infected overseas
in areas where the prevalence of the measles virus is higher than in the US,
and transmit the virus to susceptible individuals (often children) when they return. In NYC, a
substantial proportion of the cases appear to be in children too young for the vaccine.
The simple fact is that if people do not have immunity to measles, they are overwhelmingly likely to develop infection and disease following an exposure. This is a highly transmissible virus;
estimates of the basic reproduction number, R0, are as high as 18. The high degree of herd immunity in the US limits the size of outbreaks, but, as we see in the current situations in New York and California, transmission occurs due to the presence of unvaccinated persons.

In the US, all states require children to be vaccinated before starting school. However, depending on the state, children can be
exempted from the requirement for medical (notably in transplant patients and those with allergies to vaccine components), religious, or personal belief reasons. Figure 3 (shown here) of a recent
MMWR on measles transmission in the US depicts the current reasons for not receiving measles vaccination. Between January and August 2013, most measles cases (82%) were in persons who were unvaccinated. Of those, 79% cited philosophical/religious objections to vaccination as the reason for not receiving the vaccine. Outbreaks related to
religious communities are well documented in the news; recent examples include measles in
Washington State and British Columbia, measles in
New York City, and measles in
Texas.
Though this post has focused measles, there are
similar issues
with other vaccine preventable diseases, including
mumps,
pertussis, meningitis, and
others. Vaccine coverage, both in the US and overseas, must be increased if we are to decrease the incidence of such diseases. We must learn how to
more effectively communicate the benefits and risks to those who
decide against vaccination.
(image source: first graphic, Wikipedia; second & third graphics, CDC)
 After posting the piece on vaccines yesterday, a new study by BA Diep et al was brought to my attention in which the surface proteome of a prevalent strain of MRSA was determined. Work such as this is important for identifying potential antigen combinations that could be included in future multicomponent Staphylococcus aureus vaccines.
After posting the piece on vaccines yesterday, a new study by BA Diep et al was brought to my attention in which the surface proteome of a prevalent strain of MRSA was determined. Work such as this is important for identifying potential antigen combinations that could be included in future multicomponent Staphylococcus aureus vaccines.